Drug therapy problem in elderly outpatients with benign prostatic hyperplasia
Main Article Content
Abstract
Background: Benign Prostatic Hyperplasia (BPH) is a common non-malignant urological condition in ageing male. This disease is usually managed by medication and as a result, patients with BPH are exposed to Drug Therapy Problems (DTPs).
Objective: This study aimed to evaluate the prevalence and types of DTPs among elderly male with BPH in Nigeria.
Methods: A 10-year retrospective cross-sectional study was carried out among consecutively sampled elderly outpatients aged > 60 years with BPH at the Urology clinic of the Olabisi Onabanjo University Teaching Hospital, Southwest, Nigeria. The Pharmaceutical Care Network Europe Classification was used to classify DTPs. The six primary domains of Problem including adverse reactions, drug choice problem, drug use problem, interactions were explored. Drug-drug interactions (DDIs) were assessed using the Medscape® drug interaction checkers software. Chi-squared test or Fisher's exact as appropriate was used to determine associations between the domains and patients' clinical characteristics.
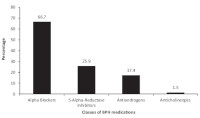
Results: A total of 201 medical records of participants, mean age 69.42 ± 7.36 years (R=60-91years) were evaluated, 35.8% had primary education and 29.9% had hypertension as comorbidity. Of the 120 DTPs (Mean ±SD; 0.6±0.2) identified among the participants, 55.8% involved DDIs, 16.7% drug choice problem and 15.0% drug use problem. Almost one-third of the DDIs (19/67; 28.4%) involved BPH medications. Co-morbidity was significantly associated with DDIs (p<0.001), drug choice problem (p<0.001) and drug use problem (p<0.001).
Conclusion: Drug therapy problems are rife among elderly patients with BPH. Drug interactions and drug choice problems, including medication non-adherence are more prevalent than other types of DTPs.
Downloads
Article Details
Issue
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
Share
References
American Urological Association (AUA) (2010) Guideline on the management of benign prostatic hyperplasia (BPH). Available:
https://www.auanet.org/guidelines/benignprostatic-hyperplasia-(bph)-guideline/benignprostatic-hyperplasia-(2010-reviewed-andvalidityconfirmed-2014) Accessed February 25, 2020.
Lee SWH, Chan EMC, Lai YK (2017). The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: A systematic review and meta-analysis. Scientific Reports 7(1):7984. doi: 10.1038/s41598-017-06628-8.
Kaplan AL (2015). Measuring the cost of care in benign prostatic hyperplasia using time-driven activity-based costing (TDABC) Healthcare 3:43-48.
Ojewola RW, Oridota ES, Balogun OS, Alabi TO, Ajayi AI, Olajide TA, et al (2017). Prevalence of clinical benign prostatic hyperplasia amongst
community-dwelling men in a South-Western Nigerian rural setting: A cross-sectional study. African Journal of Urology 23:109-115
Cindolo L, Pirozzi L, Sountoulides P, Fanizza C, Romero M, Castellan P, et al (2015). Patient's adherence on pharmacological therapy for benign prostatic hyperplasia (BPH)-associated lower urinary tract symptoms (LUTS) is different: is combination therapy better than monotherapy?. BMC Urology 15: 96. doi: 10.1186/s12894-015-0090-x
Füllhase C, Chapple C, Cornu JN, De Nunzio C, Gratzke C, Kaplan SA, et al (2013). Systematic Review of Combination Drug Therapy for Nonneurogenic Male Lower Urinary Tract Symptoms. European Urology 64 (2): 228 - 243. doi: 10.1016/j.eururo.2013.01.018.
Naslund MJ, Miner M (2007) A review of the clinical efficacy and safety of 5?-reductase inhibitors for the enlarged prostate. Clinical Therapeutics 29 (1) 17-25.
Belayneh YM, Amberbir G, Agalu A (2018). A prospective observational study of drug therapy problems in medical ward of a referral hospital in northeast Ethiopia. BMC Health Services Research 18:808. doi.org/10.1186/s12913-018-361
Pharmaceutical Care Network Europe Foundation. PCNE Classification for Drug Related problems (revised 01-05-06 Vm) V5.01 2006. Available at: https://studylib.net/doc/18191674/pcneclassification-scheme-for-drug-related-problems. Accessed September 18, 2019
Blix HS, Viktil KK, Reikvam S, Moger TA, Hjemaas BJ, Pretsch P, et al (2004). The majority of hospitalised patients have drug-related problems: results from a prospective study in general hospitals. European Journal of Clinical Pharmacology 60(9): 651-658. DOI: 10.1007/s00228-004-0830-4
Alhawassi TM, Krass I, Bajorek BV, Pont LG (2014). A systematic review of the prevalence and risk factors for adverse drug reactions in the elderly in the acute care setting. Clinical Interventions in Aging 9:2079- 2086.
Cutler RL, FernandezLlimos F, Frommer M, Benrimoj C, Garcia-Cardenas V (2018). Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open 2018;8:e016982. doi:10.1136/ bmjopen-2017-016982
Dookeeram D, Bidaisee S, Paul JF, Nunes P, Robertson P, Maharaj VR et al (2017). Polypharmacy and potential drug-drug interactions in emergency department patients in the Caribbean. International Journal of Clinical Pharmacy 39:1119-1127
Van Roozendaal BW, Krass I (2009). Development of an evidence-based checklist for the detection of drug related problems in type 2 diabetes. Pharmacy, World and Science 31: 580-595.
Eichenberger PM, Lampert ML, Kahmann IV, van Mil JWF, Hersberger KE (2010). Classification of drugrelated problems with new prescriptions using a modified PCNE classification system. Pharmacy, World and Science 32 (3) 362-372.
Zaman Huri H, Hui Xin C, Sulaiman CZ (2014). DrugRelated Problems in Patients with Benign Prostatic Hyperplasia: A Cross Sectional Retrospective Study. PLoS ONE 9 (1): e 86 215. doi:10.1371/journal.pone.0086215
Chan DC, Chen JH, Kuo HK, We CJ, Lu IS, Chiu LS, et al (2012). Drug-related problems (DRPs) identified from geriatric medication safety review clinics. Archives of Gerontology and Geriatrics 54: 168-174.
American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. Journal of American Geriatrics Society 63(11):2227- 2246.
Adibe MO, Igboeli NU, Ukwe CV (2017). Evaluation of drug therapy problems among renal patients receiving care in some tertiary hospitals in Nigeria. Tropical Journal of Pharmaceutical Research 16 (3): 697-704.
Adisa R, Osoba DO (2019). Evaluation of Drug Therapy Problems among Outpatient Hypertensive and Type-2-Diabetic Patients at a Tertiary Hospital, South-West Nigeria. Nigerian Journal of Pharmaceutical Research 15 (2):127-141.
British National Formulary 2018 Edition. British Medical Association and Royal Pharmaceutical Society.
Nivya K, Sri V, Kiran S, Ragoo N, Jayaprakash B, Sekhar MS (2015). Systemic review on drug related hospital admissions-A pubmed based search. Saudi Pharmaceutical Journal 23(1): 1-8.
Swanlund SL (2010). Successful cardiovascular medication management processes as perceived by community dwelling over age 74. Applied Nursing Research 23(1): 22-29
Drug interactions checker-Medscape drug reference Available at; https://reference.medscape.com, Accessed September 1, 2019.
Eze UIH, Oparah C, Lawal FA (2011). Identification of Drug Therapy Problems among Elderly in-patients of a Nigerian Teaching Hospital. Nigerian Journal of Pharmaceutical Research 9(1): 49-56.
Ganiyu KA, Suleiman IA, Erah PO (2014). Drug therapy problems in patients on anti-hypertensives and antidiabetic drugs in two tertiary health institutions in Niger Delta region, Nigeria. Journal of Pharmaceutical and Allied Sciences 11(1): 1986-1995.
Duan Y, Grady JJ, Albertsen PC, Helen Wu Z (2018). Tamsulosin and the risk of dementia in older men with benign prostatichyper plasia. Pharmacoepidemiology and Drug Safety 27(3):340-348.
Jiwrajka M, Yaxley W, Ranasinghe S, Perera M, Roberts MJ, Yaxley J (2018). Drugs for benign prostatic hypertrophy. Australian Prescriber 41:150-3
Huri HZ, Wee HF (2013). Drug related problems in type 2 diabetes patients with hypertension: a crosssectional retrospective study. BMC Endocrine Disorders 13:2.doi.10.1186/1472-6823-13-2.