Inhibition of potassium sensitive adenosine triphosphate channels potentiates anti-depressant activity of creatine in mice
Main Article Content
Abstract
Background: Depression is a mood disorder with poorly understood aetiology and treatment outcomes. Treatment with creatine, a nutraceutical associated with potassium sensitive adenosine triphosphate channels (KATP), produced improved results in preclinical studies of depression.
Objective: This study sought to investigate the role of KATP inhibitor and activator on the antidepressant activity of creatine in mice.
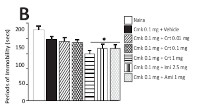
Methods: Four hundred and ninety male mice randomly allotted into groups of seven were either untreated (naïve) or pretreated with effective or sub-effective doses of glibenclamide or cromakalim, followed by selected doses of creatine, amitriptyline or imipramine for fourteen consecutive days. Groups of naïve and treated animals were thereafter subjected to forced swim test (FST) or tail suspension test (TST) or open field test (OFT).
Results: Pretreatment with effective or subeffective doses of glibenclamide and creatine, imipramine or amitriptyline significantly (p<0.05) reduced duration of immobility in the TST and FST. Conversely, cromakalim administered in combination with creatine, imipramine and amitriptyline antagonized the antidepressant effect of creatine, imipramine and amitriptyline. However, there was no difference in locomotor activity in the OFT across the treatment groups.
Conclusion: Inhibition of KATP channels potentiates the antidepressant activity of creatine.
Downloads
Article Details
Issue
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
Share
References
World Health Organization (2003). Investing in Mental Health. Department of Mental Health and Substance Dependence, Noncommunicable Diseases and Mental Health, Geneva pp 1-48.
World Health Organization (2013). Investing in Mental Health: Evidence For Action. Available at https://apps.who.int/iris/bitstream/handle
/10665/87232/ 9789241564618 eng. pdf?sequence=1.Date assessed 22nd October, 2020.
Haroz EE, Decker E, Lee C (2018). Evidence for suicide prevention and response programs with refugees: A systematic review and recommendations Geneva: United Nations High Commissioner for Refugees.
International Organization for Migration (2020). Available at; https:// publications.iom.intsystem/files/pdf/wmr_2020.pdf. Accessed 7th November, 2020.
Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR (2003). The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). Journal of the American Medical Association. 289:3095-3105.
Maoz (2007). Failure of first SSRI for depression-- what is the next step? Israel Journal of Psychiatry and Related Sciences 44(4):327-329.
Ghaemi SN (2008). Why antidepressants are not antidepressants: STEP-BD, STAR*D and the return of neurotic depression. Bipolar Disorders 10:957-968.
Ward MP, Irazoqui PP (2010). Evolving refractory major depressive disorder diagnostic and treatment paradigms: toward closed-loop therapeutics. Frontiers in Neuro engineering 3:7 doi: 10.3389/fneng.2010.00007.
Kennedy SA (2006). A review of antidepressant treatments to day. European Neuropsychopharmacology 16:S619-S623.
Sarris J, Stough C, Bousman C, Murphy J, Savage K, Smith DJ (2015a). An adjunctive antidepressant nutraceutical combination in treating major depression: study protocol, and clinical considerations. Advances in Integrative Medicine 2:49-55.
Sarris J, Logan AC, Akbaraly TN, Amminger GP, Balanza-Martinez V, Freeman MP. et al (2015b) Nutritional medicine as mainstream in psychiatry. Lancet Psychiatry 2:271-274.
Sarris J, Murphy J, Mischoulon D, Papakostas G.I, Fava M, Berk M et al (2016). Adjunctive Nutraceuticals for Depression: A Systematic Review and Meta-Analyses. American Journal of Psychiatry 173:6(575-587).
Kious BM, Kondo DG, Renshaw PF (2019). Creatine for the Treatment of Depression. Biomolecules 9(406) doi:10.3390/biom9090406.
Wyss M, Kaddurah-Daouk R (2000). Creatine and creatinine metabolism. Physiological Reviews 80:1107-1213.
Andres RH, Ducray AD, Schlattner U, Wallimann T, Widmer HR (2008). Functions and effects of creatine in the central nervous system. Brain Research Bulletin 76:329-343.
Matthews RT, Ferrante RJ, Klivenyi P, Yang L, Klein AM, Mueller G et al (1999). Creatine and cyclocreatine attenuate MPTP neurotoxicity. Experimental Neurology 157(1):142-149.
Cunha MP, Machado DG, Capra JC, Jacinto J, Bettio LE, Rodrigues ALS (2012). Antidepressant-like effect of creatine in mice involves dopaminergic activation. Journal of Psychopharmacology 26:1489-1501.
Ahn N, Leem YH, Kato M, Chang H (2016). Effects of creatine monohydrate supplementation and exercise on depression-like behaviours and raphe 5- HT neurons in mice. Journal of Exercise, Nutrition and Biochemistry 20(3):024-031.
Pazini FL, Cunha MP, Azevedo D, Rosa JM, Colla A, de Oliveira J (2017). Creatine Prevents CorticosteroneInduced Reduction in Hippocampal Proliferation and Differentiation: Possible Implication for Its Antidepressant Effect. Molecular Neurobiology 54(8):6245-6260.
Pazini FL, Cunha MP, Rodrigues ALS (2019). The possible beneficial effects of creatine for the management of depression. Progress in NeuroPsychopharmacology and Biological Psychiatry 89:193-206.
Prass K, Royl G, Lindauer U, Freyer D, Megow D, Dirnagl U et al (2007). Improved reperfusion and neuroprotection by creatine in a mouse model of stroke. Journal of Cerebral Blood Flow and Metabolism 27:452-459.
Crawford RM, Ranki HJ, Botting CB, Budas GR, Jovanovic A (2002). Creatine kinase is physically associated with the cardiac ATP-sensitive K+ channel in vivo. Federation of American Societies for Experimental Biology Journal 16(1):102-104.
Selivanov VA, Alekseev AE, Hodgson DM, Dzeja PP, Terzic A (2004). Nucleotide-gated KATP channels integrated with creatine and adenylate kinases: Amplification, tuning and sensing of energetic signals in the compartmentalized cellular environment. Molecular and Cellular Biochemistry 256-257(1-2):243-256.
Thomzig A, Laube G, Pruss H, Veh RW (2005). Poreforming subunits of K-ATP channels, Kir6.1 and Kir6.2, display prominent differences in regional and cellular distribution in the rat brain. Journal of Comparative Neurology 484:313-330.
Nazari SK, Nikoui V, Ostadhadi S, Chegini ZH, Oryan S, Bakhtiarian A (2016). Possible Involvement of ATPsensitive Potassium Channels in the AntidepressantLike Effect of Baclofen in Mouse Forced Swimming Test. Pharmacology Reports 68(6):1214-1220.
Naserzadeh R, Abad N, Ghorbanzadeh B, Dolatshahi M, Mansouri MT (2019). Simvastatin exerts antidepressant-like activity in mouse forced swimming test: Role of NO-cGMP-KATP channels pathway and PPAR-gamma receptors. Pharmacology Biochemistry and Behaviour 180:92?100.
Shakiba S, Rezaee M, Afshari K, Kazemi K, Sharifi K, Haddadi N et al (2019). Evaluation of the pharmacological involvement of ATP-sensitive potassium (KATP) channels in the antidepressant-like effects of topiramate on mice. Naunyn Schmiedebergs Archives of Pharmacology 392(7):833?842.
Kobayashi T, Washiyama K, Ikeda K (2006). Inhibition of G protein-activated inwardly rectifying K+ channels by the antidepressant paroxetine. Journal of Pharmacological Sciences 102 (3)278-287.
Donato F, Filho CB, Giacomeli R, Alvater EET, Del Fabbro L, Antunes MS et al (2015). Evidence for the Involvement of Potassium Channel Inhibition in the Antidepressant-Like Effects of Hesperidin in the Tail Suspension Test in Mice. Journal of Medicinal Food 18(7):818-823
NIH, Public Health Service Policy on Humane Care and Use of Laboratory Animals, 2015. http://grants.nih.gov/grants/olaw/ references/PHS Policy Lab Animals.pdf.
Steru L, Chermat R, Thierry B, Simon P (1985). Tail suspension test: a new method for screening antidepressants in mice. Psychopharmacology 85:367-370.
Porsolt RD, Bertin A, Jalfre M (1977). Behavioral despair in mice: a primary screening test for antidepressants. Archives Internationales de Pharmacodynamie et de Therapie 229:327-336.
Kordjazy N, Haj-Mirzaian A, Amiri S, Ostadhadi S, Kordjazy M, Sharifzadeh M et al (2015). Elevated Levels of nitric oxide mediates the anti-depressant effect of rubidium chloride in mice. European Journal of Pharmacology 762:411-418.
Carola V, D'Olimpio F, Brunamonti E, Mangia F, Renzi P (2002). Evaluation of the elevated plus-maze and open-field tests for the assessment of anxiety related behaviour in inbred mice. Behavioural Brain Research 134: 49-57.
Choleris E, Thomas AW, Kavaliers M, Prato FS (2001). A detailed ethological analysis of the mouse open field test: effects of diazepam, chlordiazepoxide and an extremely low frequency pulsed magnetic field. Neuroscience and Biobehavioural Reviews 25: 235-260.
Bortolatto CF, Jesse CR, Wilhelm EA, Nogueira CW (2010). Involvement of potassium channels in the antidepressant-like effect of venlafaxine in mice. Life Sciences 86:372-376.
Cunha MP, Pazini FL, Oliveira A, Machado, Lucia SA (2013). Evidence for the involvement of 5-HT1A receptor in the acute antidepressant-like effect of creatine in mice. Brain Research Bulletin 95:61-69.
Porsolt RD (2000). Animal models of depressing: utility for transgenic research. Review of Neuroscience 11:53-58.
Cryan JF, Markou A, Lucki I (2002) Assessing antidepressant activity in rodents: recent developments and future needs. Trends in Pharmacological Sciences 23:238-245.
O'Leary OF, Cryan JF (2009). The tail-suspension test: a model for characterizing antidepressant activity in Mice. Neuromethods 42:119-137
Schechter LE (1997). The potassium channel blockers 4-aminopyridine and tetraethylammonium increase the spontaneous basal release of [3H]5- hydroxytryptamine in rat hippocampal slices. The Journal of Pharmacology and Experimental Therapeutics 282 (1):262-270.
Sun XL, Hu G (2010). ATP-sensitive potassium channels: a promising target for protecting neurovascular unit function in stroke. Clinical and Experimental Pharmacology and Physiology 37:243-252.
Sun H, Feng Z (2013). Neuroprotective role of ATPsensitive potassium channels in cerebral ischemia Acta Pharmacologica Sinica 34:24-32.
Castagné V, Porsolt RD, Moser P (2009). Use of latency to immobility improves detection of antidepressant-like activity in the behavioral despair test in the mouse. European Journal of Pharmacology 15;616(1-3):128-33.