Investigation of herb-drug interaction between MAMA powder herbal antimalarial remedy and amodiaquine, chloroquine, artesunate in murine malaria Étude de l'interaction plante-médicament entre le remède antipaludique à base de plantes en <i>poudre MAMA</i> et l'amodiaquine, la chloroquine et l'artésunate dans le cas du paludisme murin
Main Article Content
Abstract
ENGLISH
Background: Antimalarial herbal remedies are traditionally presented as infusions, decoctions and extracts. There is limited information on antimalarial herbal powder presentations. The outcomes of possible co-administration of MAMA POWDER (MP), a herbal powder listed for malaria treatment, with orthodox antimalarial drugs, had not been explored.
Objectives: This study investigated MP as a reduced particle-sized powder, and its effects on amodiaquine (AQ), chloroquine (CQ), artesunate (AS) in mice.
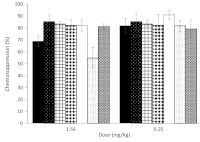
Methods: MAMA POWDER comprises the powdered stem bark of Alstonia boonei De Wild (Apocynaceae) and seed of Picralima nitida H Durand (Apocynaceae). The barks were milled, sieved (particle size, 180 μm), mixed and suspended in propylene glycol (50 %). This suspension was assessed on chloroquine-sensitive and chloroquine-resistant Plasmodium berghei strains in varying oral doses (0.39-100 mg/kg), using the chemosuppressive and curative antimalarial test models. Co-administration of MP with the orthodox drugs was similarly investigated as follows: (MP 1.56+AQ 10; MP 6.25+AQ 10), (MP 1.56+CQ 10; MP 6.25+CQ 10), (MP 1.56+AS 4; MP 6.25+AS 4)
mg/kg.
Results: MP suspension (6.25 mg/kg) exhibited considerable antimalarial chemosuppression (82 %) and it enhanced the activity of AQ (MP 6.25+AQ 10 mg/kg) in chloroquine-sensitive malaria infection (91 %). Significant antagonistic interactions were observed with the combinations of MP (1.56 mg/kg, 69%) and CQ (55.2 %) respectively.
Conclusion: MP exhibited significant antimalarial activity. The potentiation of AQ and antagonism with CQ, suggested herb-drug interactions, which called for further investigation.
FRENCH
Contexte: Les remèdes antipaludiques à base de plantes se présentent traditionnellement sous forme d'infusions, de décoctions et d'extraits. Les informations sur les présentations de poudres antipaludiques à base de plantes sont limitées. Les effets d'une éventuelle co-administration de MAMA POWDER (MP), une poudre à base de plantes indiquée pour le traitement du paludisme, avec médicaments antipaludiques orthodoxes n'ont pas été étudiés.
Objectifs: Par conséquent, cette étude a examiné le MP sous forme de poudre de taille de particules réduite et ses effets sur l'amodiaquine (AQ), la chloroquine (CQ) et l'artésunate (AS) chez la souris.
Méthodes: MAMA POWDER comprend l'écorce de tige en poudre d'Alstonia boonei De Wild ( Apocynacées) et la graine de Picralima nitida H Durand (Apocynacées). Les écorces ont été broyées, tamisées (granulométrie : 180 µm), mélangées et mises en suspension dans du propylène glycol (50%). Cette suspension a été évaluée sur des souches de Plasmodium berghei sensibles et résistantes à la chloroquine à différentes doses orales (0,39-100mg/kg), en utilisant les modèles de test antipaludique chimiosuppresseur et curatif. La co-administration de MP avec les médicaments orthodoxes a également été étudiée de la manière suivante : (MP 1,56 + AQ 10 ; MP 6,25 + AQ 10), (MP 1,56 + CQ 10 ; MP 6,25 + CQ 10), (MP 1,56 + AS 4 ; MP 6,25 + AS 4) mg/kg.
Résultats: La suspension de MP (6,25 mg/kg) a montré une chimio-suppression antipaludique considérable (82%) et a amélioré l'activité de l'AQ (MP 6,25 + AQ 10 mg/kg) dans l'infection paludique sensible à la chloroquine (91%). Des interactions antagonistes significatives ont été observées avec les combinaisons de MP (1,56 mg/kg, 69 %) et de CQ (55,2 %) respectivement.
Conclusion: Le MP a montré une activité antipaludique significative. La potentialisation de l'AQ et l'antagonisme avec la CQ ont suggéré des interactions entre les plantes et les médicaments, ce qui nécessite des recherches plus approfondies.
Downloads
Article Details
Issue
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
Share
References
1. World Health Organisation (2024) World Malaria Report. Geneva, Switzerland, World Health Organisation, Available at 2024 highlights from the WHO Global Malaria Programme. Accessed on 22nd February 2025
2. James PB, Wardle J, Steel A, Adams J. (2018) Traditional, complementary and alternative medicine use in Sub-Saharan Africa: a systematic review. BMJ Global Health 3:e000895 https://doi.org/10.1136/bmjgh-2018-000895
3. Ajayi CO, Elujoba AA, Adepiti AO. (2015) Antiplasmodial properties of Alstonia boonei stembark and Picralima nitida seed in different
combinations. Nigeria Journal of Natural Products and Medicine. 19:71-77
4. Ajayi CO, Elujoba AA, Adepiti AO, Bejide RA, Adeyemi OI. (2020) Neuro-behavioural and Repeated-Dose Toxicity studies on the extractive from the decoction of a mixture of Alstonia boonei and Picralima nitida in mice. Comparative Clinical Pathology. 29: 375-383.
5. Adeyoju EO, Ajayi CO, Adepiti AO, Elujoba AA. (2022) Comparative in vivo antimalarial activities of aqueous and methanol extracts of MAMA powder-A herbal antimalarial preparation. Journal of Ethnopharmacology. doi:10.1016/j.jep.2021.114686
6. Qihua L, Jin W, Zhiping P, Fenglin L, Xiaolin T (2015) Review of the powder and decoction formulae in Traditional Chinese Medicine based on pharmacologically active substances and clinical evidence. Journal Traditional Chinese Medicine.35:355-360.
7. Zaigham H, Tauheed A, Ali A. (2019). Recent trend in traditional medicine dosage form and present status of Unani and Ayurvedic medicine. International Journal of Pharmaceutical Science & Research, 10(4): 1640-49.
8. Kumadoh DO, Ofori-Kwakye KW. Dosage forms of herbal medicinal products and their stability considerations-an overview (2017). Journal of Critical Review.;4(4):1-8.
9. Adepiti AO, Elujoba AA, Bolaji OO. (2016) Evaluation of herbal antimalarial MAMA decoction-amodiaquine combination in murine malaria model. Pharmaceutical Biology. 54: 2298-2303.
10. National Research Council. Guide for the Care and Use of Laboratory Animals 8th edn., WashingtonNational Academies Press (US), 2011
11. Adeyemo-Salami O A, Ademowo OG, Farombi EO. (2020). Antioxidant and antiplasmodial activities of methanol leaf extract of Paullinia pinnata. Journal of Herbs Spices and Medicinal Plants, 26: 315-328.
12. OECD (Organisation for Economic Co-operation and Development). OECD Guidelines for the Testing of Chemicals, Section 4, Test No. 423: Acute Oral Toxicity - Acute Toxic Class Method. 2001
13. Peters W, Fleck SL, Robinson BL, Stewart LB, Jefford CW. (2002) The chemotherapy of rodent malaria. LX. The importance of formulation in evaluating the blood schizontocidal activity of some endoperoxide antimalarials. Annals of Tropical Medicine and Parasitology. 96: 559-573.
14. Ryley JF, Peters W. (1970) The antimalarial activity of some quinolone esters. Annals of Tropical Medicine and Parasitology. 64: 209-222.
15. Byeon JC, Ahn JB, Jang WS, Lee SE, Choi JS et al. (2019) Recent formulation approaches to oral delivery of herbal medicines. Journal of
Pharmaceutical Investigation. 49:17-26.
16. Zhi H, Li Z, Deng Y, Qi P, Hou J et al. (2019) Comparative in vivo constituents and pharmacokinetic study in rats after oral administration of ultrafine granular powder and traditional decoction slices of Chinese Salvia. Biomedical Chromatography. doi:10.1002/bmc.4385
17. Iwu MM, Klayman DL, Jackson JE, Tally JD, Andersen SL (1994) Alkaloids of Picralima nitida used for treatment of protozoal diseases. United States Patent US 5,290,553.
18. Onaku LO, Attama AA, Okore VC, Tijani AY, Ngene AA et al. (2011) Antagonistic antimalarial properties of pawpaw leaf aqueous extract in combination with artesunic acid in Plasmodium berghei-infected mice. Journal of Vector Borne Diseases. 48: 96-100.
19. Agbedahunsi JM, Adepiti AO, Adedini AA, Akinsomisoye A, Adepitan O. (2016) Antimalarial properties of Morinda lucida and Alstonia boonei on Sulphadoxine-Pyrimethamine and Curcuma longa on Quinine in mice. Journal of Herbs Spices and Medicinal Plants, 22:1-10
20. Issa FH, Al-Habori M, Chance ML. (2016) Effect of khat (Catha edulis) use on the bioavailability, plasma levels, and antimalarial activity of chloroquine. Sultan Qaboos University Medical Journal 16(2):e182-188.
21. Obinna E. (2010) Antimalarial activity of Ageratum conyzoides in combination with chloroquine and artesunate. Asian Pacific Journal of Tropical Medicine. 3:943-947.
22. Aina O O, Agomo C O, Adekilekun H H, Kareem K O, Okoyenta CO, Bamgbose DJ. (2024) In vivo antimalarial activity of Yoyo bitters®, a polyherbal formulation against Plasmodium berghei in Swiss mice. West African Journal of Pharmacy. 35(2): 57-65.