A case-control study assessing estrogen-progesterone ratio as a biomarker of epilepsy in women
Main Article Content
Abstract
Background: The relationship between sex hormones and epilepsy has been explored with studies showing a bidirectional relationship. However, none has focused on potential use of Estrogen/Progesterone Ratio (EPR) as apossible promising biomarker of epilepsy.
Objective: The aim of this study was to determine the association between epilepsy and EPR among women and possible utilization as a biomarker.
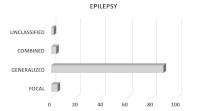
Methods: This is a case-control cross sectional study consisting of randomly and purposefully selected 200 women in which 100 were Women with Epilepsy (WoWE) while the remaining 100 were Women Without Epilepsy (WoWoE) (i.e control). The 100 WoWE were randomly divided into two groups (with 50 each on Carbamazepine (CAR) and Levetiracetam (LVC) group). The diagnosis of epilepsy were in accordance with 2017 International League Against Epilepsy (ILAE) and supported by Electroencephalographic features. Statistical Package for Social Science (SPSS) version 22 was used for data analysis. Hormone sample collection was based on Enzyme Linked Immunosorbent Assay (ELISA) principles.
Results: There was higher Follicular Phase EPR(FP-EPR) [139.87±298.11 vs 50.65±54.21; p0.040], and higher Luteal Phase EPR(LP-EPR) [135.15±40.03 vs 40.03±37.70; p0.012] in WoWE compared to WoWoE. There was higher FP-EPR [173.25±399.57 vs 50.64±54.20; p0.036], and higher LP-EPR [171.36±354.00 vs 40.03±37.70; p0.011] in CAR group compared to control. There was also a significantly higher LP-EPR level among cases on LVC group compared to control [99.66±115.16 vs 40.03±37.70; p0.001]. There was no difference in the FP-EPR and LPEPR between CAR and LVC groups [173.25±399.87 vs 106.49±132.10; p0.275], [171.36±354.00 vs 99.66±115.16; p0.177].
Conclusion: There was a higher level of EPR in cases compared to control, however the EPR was comparable in cases on CAR and LVC. EPR might be a promising biomarker of epilepsy.
Downloads
Article Details
Issue
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
Share
References
Fisher RS (2017). An overview of the 2017 ILAE operational classification of seizure types. Epilepsy Behav 70: 271-273.
Pennell PB (2009). Hormonal aspects of epilepsy. Neurol Clin 27: 941-965.
Verrotti A, D'Egidio C, Coppola G, Parisi P, Chiarelli F (2009). Epilepsy, sex hormones and antiepileptic drugs in female patients. Expert Rev Neurother 9: 1803-1814.
Shiono S, Williamson J, Kapur J, Joshi S (2019). Progesterone receptor activation regulates seizure susceptibility. Ann Clin Transl Neurol 6: 1302-1310.
Amini L, Hematian M, Montazeri A, Gharegozli K (2018). Comparing the frequency of polycystic ovary syndrome in women with and without epilepsy. Journal Family Med Prim Care 7: 16-20.
Reddy DS (2013). Neuroendocrine aspects of catamenial epilepsy. Horm Behav 63: 254-266.
Harden CL, Pennell PB (2013). Neuroendocrine considerations in the treatment of men and women with epilepsy. Lancet Neurol 12: 72-83.
Svalheim S, Taubøll E, Luef G, Lossius A, Rauchenzauner M, Sandvand F, Bertelsan M, Morkind L, Gjerstad L (2009). Differential effects of
levetiracetam, carbamazepine, and lamotrigine on reproductive endocrine function in adults. Epilepsy Behav 16: 281-287.
Ogunjimi L, Yaria J, Makanjuola A, Alabi A, Osalusi B, Oboh D, Olusola-Bello M, Olawale O, Ogunniyi A (2021). Polycystic ovarian syndrome in Nigerian women with epilepsy on carbamazepine/levetiracetam monotherapy. Acta Neurol Scand 143: 146-153.
Hirsch LJ, LaRoche SM, Gaspard N, Gerard E, Svoronos A, Herman ST, Mani R, Arif H, Jette N, Minazad Y, Kerrigan JF, Vespa P, Hantus S, Classen J, Young GB, So E, Kaplan PW, Nuwer MW, Fountain NB, Drislane FW(2013). American Clinical Neurophysiology Society's Standardized Critical Care EEG Terminology: 2012 version. Journal Clin Neurophysiol 30: 1-27.
Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, Engel Jr J, Forsgren L, French JA, Glynn M, Hesdorffer DC, Lee BI, Mathern GW, Moshe SL, Perucca E, Scheffer, IE, Tomson T, Watanabe M, Wiebe S (2014). ILAE official report: a practical clinical definition of epilepsy. Epilepsia 55: 475-482.
Fadare JO, Sunmonu TA, Bankole IA, Adekeye KA, Abubakar SA (2018). Medication adherence and adverse effect profile of antiepileptic drugs in Nigerian patients with epilepsy. Neurodegener Dis Manag 8: 25-36.
Verrotti A, Lattanzi S, Brigo F, Zaccara G (2020). Pharmacodynamic interactions of antiepileptic drugs: From bench to clinical practice. Epilepsy Behav 104: 106939.
Meador KJ, Penovich P, Baker GA, Pennell PG, Bromfield E, Pack A, Liporace, JD, Sam M, Kalayjian LA, Thurman DJ, Moore E, Loring DW (2009). Antiepileptic drug use in women of childbearing age. Epilepsy Behav 15: 339-343.
Abou-Khalil BW (2016). Antiepileptic Drugs. Continuum (Minneap Minn) 22: 132-156.
Chakravarthi S, Goyal MK, Modi M, Bhalla A, Singh P, (2015). Levetiracetam versus phenytoin in management of status epilepticus. Journal Clin Neurosci 22: 959-963.
Olusanya A, Ogunleye O, Godman B, Fadare J, Danesi M (2017). Adverse effects of carbamazepine monotherapy among patients in Nigeria: a pilot study and implications. Journal Comp Eff Res 6: 33- 42.
Bauer J, Isojärvi JIT, Herzog AG, Reuber M, Polson D, Taubøll E, Genton P, Ven HV, Roesing B, Luef GJ, Galimberti CA, Parys JV, Flügel D, Bergmann A, Elger CE (2002). Reproductive dysfunction in women with epilepsy: recommendations for evaluation and management. Journal Neurol Neurosurg Psychiatry 73: 121-125.
Herzog AG, Coleman AE, Jacobs AR, Klein P, Friedman MN, Drislane FW, Ransil BJ, Schomer DL (2003). Interictal EEG discharges, reproductive hormones, and menstrual disorders in epilepsy. Ann Neurol 54: 625-637.
Hamson DK, Roes MM, Galea LAM (2016). Sex Hormones and Cognition: Neuroendocrine Influences on Memory and Learning. Compr Physiol 6: 1295-1337. 21. Lebrun CEI, van der Schouw YT, de Jong FH, Pols HAP, Grobbee DE, Lamberts SWJ (2005).. Endogenous oestrogens are related to cognition in healthy elderly women. Clin Endocrinol (Oxf) 63: 50-55.
Maguire MJ, Nevitt SJ (2019). Treatments for seizures in catamenial (menstrual-related) epilepsy. Cochrane Database Syst Rev 10: CD013225.
Reimers A, Brodtkorb E, Sabers A (2015). Interactions between hormonal contraception and antiepileptic drugs: Clinical and mechanistic considerations. Seizure 28: 66-70.
Velíšková J, DeSantis KA (2013). Sex and Hormonal influences on Seizures and Epilepsy. Horm Behav 63: 267-277.
Ogunjimi L, Yaria J, Makanjuola A, Alabi A, Osalusi B, Oboh D, Olusola-Bello M, Aderinola A, Ogunniyi A (2021) Cognitive dysfunction in Nigerian women with epilepsy on carbamazepine and levetiracetam monotherapy. Brain Behav e02038.
Svalheim S, Taubøll E, Surdova K, Ormel L, Dahl E, Aleksandersen M, McNeilly A, Gjerstad L, Ropstad E (2008). Long-term levetiracetam treatment affects reproductive endocrine function in female Wistar rats. Seizure 17: 203-209.
Wu T, Chen C-C, Chen T-C, Tseng Y-F, Chiang C-B, Hung C-C, Liou H-L (2009). Clinical efficacy and cognitive and neuropsychological effects of levetiracetam in epilepsy: an open-label multicenter study. Epilepsy Behav 16: 468-474.
Ag H (2006). Menstrual Disorders in Women With Epilepsy. Neurology; 66. DOI: 10.1212/wnl.66.66_suppl_3.s23.
Isojärvi JIT, Taubøll E, Herzog AG (2005). Effect of antiepileptic drugs on reproductive endocrine function in individuals with epilepsy. CNS Drugs 19: 207-223.