Chemotherapeutic potentials of aqueous Securinega virosa leaf extract in benzene-induced leukaemic mice
Main Article Content
Abstract
Background: Securinega virosa (common bushweed; Chinese waterberry) is a widely distributed plant throughout tropical Africa and China, but can also be found in India, Malaya, and Australia. The leaves are used traditionally to treat fever, body pain, stomach ache, rheumatism, epilepsy, infectious and chronic diseases including diabetes and cancer due to the presence of phytochemicals of therapeutic importance.
Objective: This study investigated the anti-leukaemic and chemopreventive properties of aqueous Securinega virosa leaf extracts in benzene-induced leukaemia.
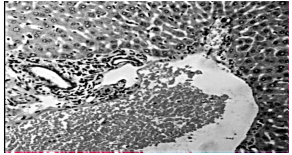
Methods: Forty male Swiss mice (weight range 15-32g) categorised into control (8) and test (32) groups were used. Leukaemia was induced in the test group using 400 mg/kg body weight benzene. Blood film was prepared and examined microscopically for the presence of blast cell to confirm leukaemia. For therapeutic studies, Securinega virosa extract was administered for a period of three weeks after blood was obtained for haematological studies and film preparation. Bone marrow extraction and liver tissue excision were done for microscopic and histopathological studies. Liver tissue malondialdehyde (MDA) and catalase levels were also determined.
Results: showed the presence of blast cells in the blood and BM; and revealed a significant increase (p < 0.05) in percentage blast cells, percentage micronucleated polychromatic erythrocytes, leukocyte counts, erythrocyte count and liver MDA; and a significant decrease (p < 0.05) in haemoglobin concentration, haematocrit, platelet count, and liver catalase activities amongst leukaemic-untreated groups when compared to Securinega virosa extract-treated groups.
Conclusion: The anti-leukaemic potentials and chemopreventive activity of aqueous Securinega virosa extract is hereby inferenced as indicated by improvements in haematological parameters, markers of oxidative stress, and the general liver cyto-architecture described by well-organised portal triad and well distributed hepatocytes among the extract-treated mice.
Downloads
Article Details
Issue
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
Share
References
1. Kaseb H, Madan A, Killeen RB, Hozayen S. (2023) TCell Prolymphocytic Leukemia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing;.
2. Hutter JJ (2010). Childhood leukemia." Pediatrics in review/American Academy of Pediatrics 31(6): 234-241.
3. Bispo JAB, Pinheiro PS, Kobetz EK (2020). Epidemiology and Etiology of Leukemia and Lymphoma. Cold Spring Harbor Perspectives Medicine 10 (6).
4. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021). Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer Journal for Clinicians 71(3): 209-249.
5. National Cancer Institute. Cancer Stat Facts: Leukemia, 2021. Available Online. Accessed, 26/07/2021.
6. Dombret H, Gardin C (2016). An Update of Current Treatments for Adult Acute Myeloid Leukemia. Blood 127(1): 53-61.
7. Cosa P, Vlietinck AJ, Berghe DV, Maes L (2006). Antiinfective potential of natural products: How to develop a stronger in vitro 'proof-of-concept'. Journal Ethnopharmacology 106: 290-302.
8. Tatematsu H, Mori M, Yang TH, Chang JJ, Lee TT, Lee KH (1991). Cytotoxic principles of Securinega virosa: virosecurininie and viroallosecurinine and related derivatives. Journal Pharmaceutical Science 80: 325-327.
9. Neuwinger JD. (1996) Translated from by Porter A. African ethnobotany poison and drugs. Chapman and Hall: Weinheim, 495-499.
10. Duraipandiyan V, Ayyanar M, Ignacimuthu S (2006). Antimicrobial activity of some ethno-medicinal plants used by Paliyar tribe from Tamil Nadu, India. BMC Complementary Alternative Medicine. 6: 35-41.
11. Magaji MG, Yaro AH, Musa AM, Anuka JA, AbduAguye I, Hussaini IM (2012). Central depressant activities of butanol fraction of Securinega virosa root back in mice. Journal of Ethnopharmacology 141(1): 128-133.
12. Danlami U, David BM, Joyce OO, Olutayo O, Thomas SA (2013). The Antioxidant Potentials and Phytochemical Properties of the Hexane, Ethyl acetate and Ethanolic Extracts of Securinega virosa (Euphorbiaceae) Leaves. Journal of Applied Pharmaceutical Science 3(05): 131-133.
13. Magaji MG, Anuka JA, Abdu-Aguye I, Yaro AH, Hussaini IM (2008a13). Behavioural effects of the methanolic root bark extract of Securinega virosa in rodents. African Journal Traditional Complement Alternative Medicine. 5(2): 147-153.
14. Magaji MG, Anuka JA, Abdu-Aguye I, Yaro AH, Hussaini IM (2008b). Preliminary studies on antiinflammatory and analgesic activities of Securinega virosa (Euphorbiaceae) in experimental animal model. Journal of Medicinal Plants Research 2(2): 039-044.
15. Salawu MO, Yekeen A, Nafiu MO, Oloyede HO (2019). Anti-Ulcerogenic Potential of Aqueous Extract of Securinega virosa Leaf in IndomethacinInduced Ulcerated Rats. Notulae Scientia Biologicae 11(2): 196-204.
16. Soladoye MO, Amusa NA, Raji-Esan SO, Chukwuma EC, Taiwo AA (2010). Ethnobotanical Survey of AntiCancer Plants in Ogun State, Nigeria. Annual Biological Research International 1(4): 261-273.
17. Magaji MG, Ya'u J, Musa AM, Anuka JA, Abdulquadir I, Hussaini IM (2015). Securinega virosa (Euphorbiaceae) root bark extract inhibits glioblastoma multiforme cell survival in vitro, African Journal of Pharmacy and Pharmacology 9(27): 684-693.
18. Amenu J, Neglo D, Abaye D (2019). Comparative Study of the Antioxidant and Antimicrobial Activities of Compounds Isolated from Solvent Extracts of the Roots of Securinega virosa. Journal of Biosciences and Medicines 7: 27-41.
19. National Research Council. Guide for the care and use of laboratory animals 8th edn. National Academy Press, Washington, DC, 2011:41-81.
20. Lau A, Belanger CL, Winn LM (2019). In utero and acute exposure to benzene: Investigation of DNA double-strand breaks and DNA recombination in mice. Mutation Research 676(1-2): 74-82.
21. Liu X, Quan N. (2015). Immune Cell Isolation from Mouse Femur Bone Marrow. Biologicae Protoc 5(20): e1631.
22. Pearse AE. (1985) Histochemistry. Theoretical and Applied Analytical Technology. Edinburgh: ChurchillLivingstone, 1012-1026.
23. Iyiola S, Avwioro OG (2011). Alum haematoxylin stain for the demonstration of nuclear and extra nuclear substances. Journal of Pharmacy and Clinical Sciences 32: 197-199.
24. Varshney R, Kale RK (1990). Efffect of calmodulin antagonist on radiation-induced lipid peroxidation in microsomes. International Journal of Radiation Biology 58: 733-743.
25. Gott L (1991). A simple method for determination of serum catalase activity and revision of reference range. Clinical Chim Acta 196(2-3): 143-151.
26. Ola SO, Ogunkanmbi EO, Opeodu EB (2022). Chemoprotection by Kolaviron of Garcinia kola in Benzene-induced leukemogenesis in Wistar rats, Egyptian Journal of Basic and Applied Sciences 9: 1, 151-161.
27. Suzuki Y, Nagae Y, Li J, Sakaba H, Mozawa K, Takahashi A, Shimizu H (1989). The micronucleus test and erythropoiesis. Effects of erythropoietin and a mutagen on the ratio of polychromatic to normochromatic erythrocytes (P/N ratio). Mutagenesis 4(6): 420-4.
28. Gao X, Wang Y, Zhang I, Lin L, Yao Q, Xiang G (2017). Bergenin suppresses the growth of colorectal cancer cells by inhibiting PI3K/AKT/mTOR signaling pathway. Tropical Journal of Pharmaceutical Research 16(10): 2307-2313.
29. Shi X, Xu M, Luo K, Huang W, Yu H, Zhou T (2019). Anticancer activity of bergenin against cervical cancer cells involves apoptosis, cell cycle arrest, inhibition of cell migration and the STAT3 signalling pathway. Experimental and Therapeutic Medicine 17(5): 3525-3529.
30. Adewoyin AS, Nwogoh B (2014). Peripheral blood film - a review. Annals Ibadan Postgraduate Medicine 12(2): 71-79.
31. Chen H, Eastmond DA (1995). Topoisomerase inhibition by phenolic metabolites: a potential mechanism for benzene's clastogenic effects. Carcinogenesis 16(10): 2301-2307.
32. Ghosh S, Advani SH (2005). T-cell prolymphocytic leukemia- a rare case. Indian Journal Cancer 42(2): 104-106.
33. O'Connell KE, Mikkola AM, Stepanek AM, Vernet A, Hall CD, Sun CC, Yildirim E, Staropoli JF, Lee JT, Brown DE (2015). Practical murine hematopathology: a comparative review and implications for research. Comparative Medicine 65(2): 96-113.
34. Dong C, Zhang NJ, Zhang LJ (2021). Oxidative stress in leukemia and antioxidant treatment. Chinese Medicine Journal (Engl) 134(16): 1897-1907.